It is a dream of every medical student to one day be able to put a stethoscope on a patient and listen to their heart sounds, and this time correctly interpret it as well. In this article, we will go through the basics of how to auscultate (“Listening the sounds of internal organs from outside in an non-invasive manner”) heart sounds. In the upcoming posts, we will try to address the murmurs in detail.
STETHOSCOPE :
Stethoscope is like an ornament for medical professionals and rightly so, It used to be one of the only tools to be able to diagnose complex medical conditions on the outpatient basis in a non-invasive manner. For a medical student of our generation, a stethoscope might not mean as much due to the invention of advanced diagnostics which are faster, far more accurate, objective in making decisions and becoming widely available. Still, auscultation is a primary care level practice widely used to screen patients for the presence of various conditions and in some cases, diagnose it.
PARTS OF A STETHOSCOPE :
We will take a look at parts of the stethoscope for the starters.
It mainly has following three parts :
1). Earpiece
2). Connecting PVC tubing
3). Chest piece (Has a larger part called Diaphragm and a smaller part called Bell)
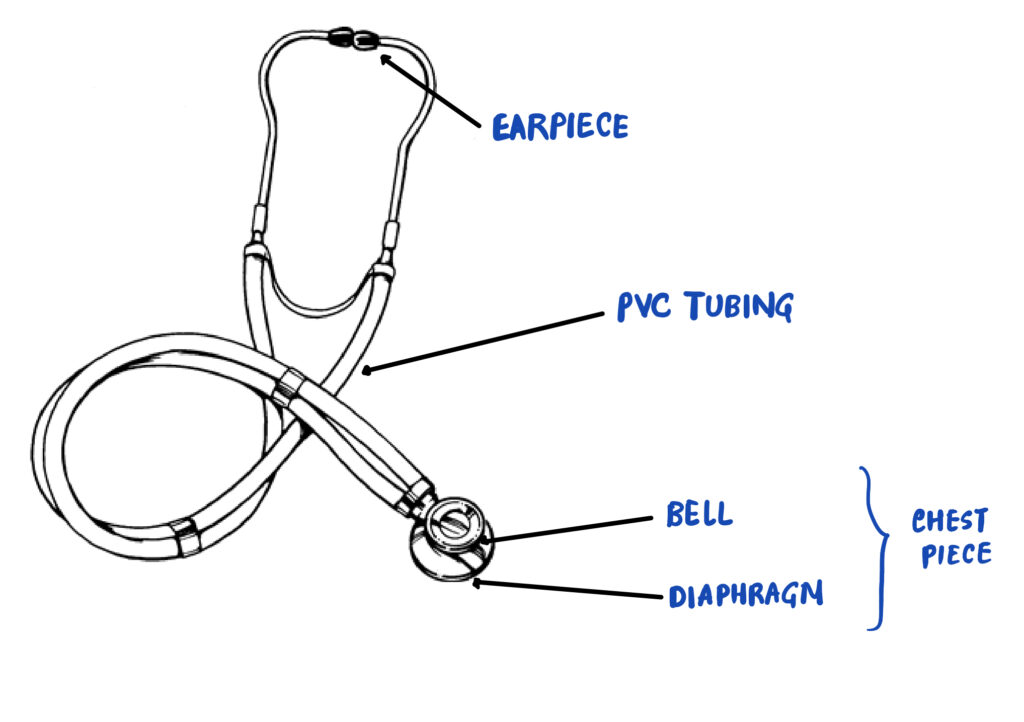
Chest Piece has two distinct parts which are meant to be used when detecting different pitched sounds.
Low pitch sounds : Bell (Diaphragm can also detect low pitch sounds to a lesser degree)
High pitch sounds : Diaphragm
HOW TO HOLD A STETHOSCOPE? :
Let’s first learn how to hold a stethoscope before starting discussion on auscultation findings.

Stethoscope is usually held with the neck connecting the diaphragm and the bell in between index and middle finger, as shown in the image below. Although it can vary as per Health Practitioner’s individual preference.
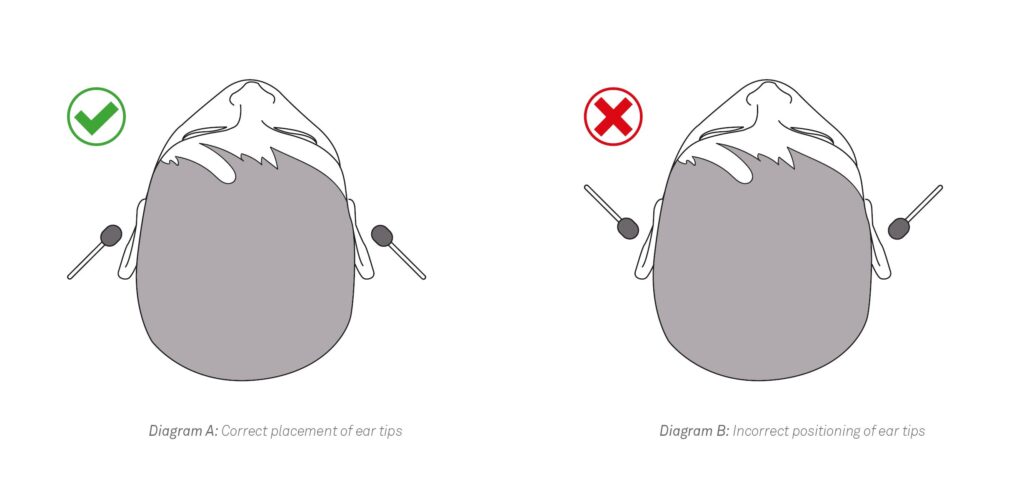
Ear tips should be directed medially and forwards when in hand in order to minimise the tension in the ears. (You should not be able to see the holes in the tips when in the hand.)
Care has to be taken not to press too much or too lightly while auscultation with a stethoscope. It just needs to be gentle enough so that you can appreciate the heart sounds.
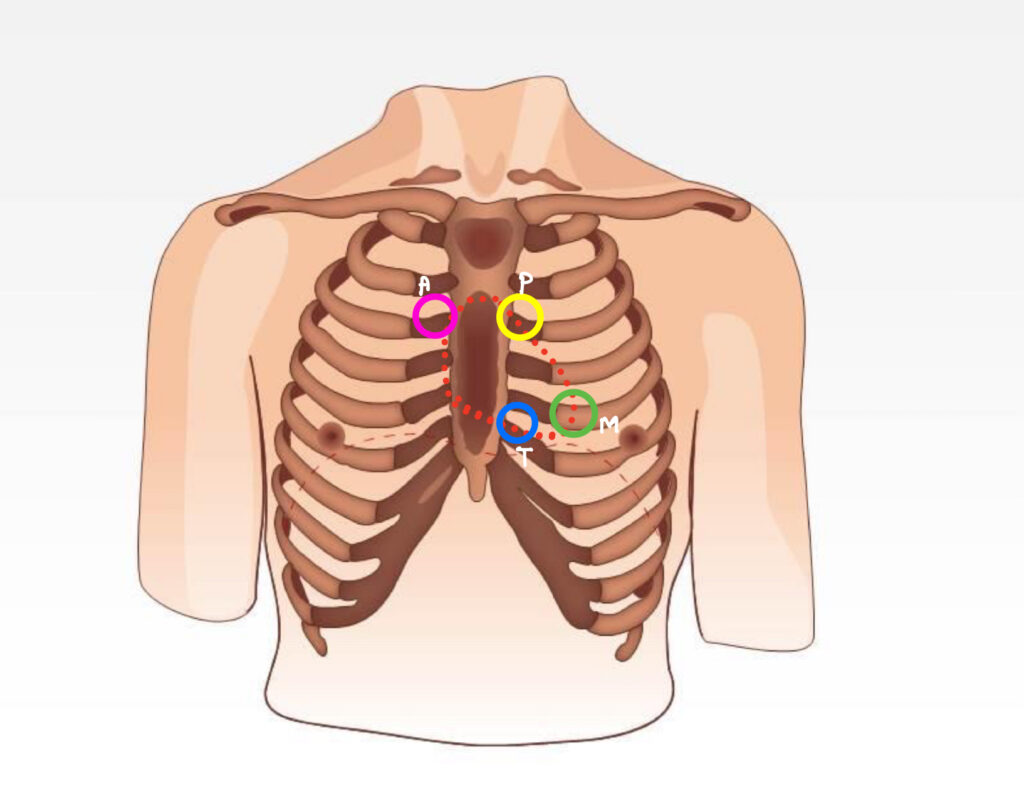
AREAS TO AUSCULTATE :
There are four areas to auscultate in a cardiac examination :
1). Mitral Area : Midclavicular line in 5th intercostal space (ICS)
2). Tricuspid Area : Lower left sternal border, 5th ICS
3). Aortic Area : Upper right sternal border, 2nd ICS
4). Pulmonary Area : Upper left sternal border, 2md ICS
These areas reflect the position of the valve of the corresponding name. In theory, they correspond to the area of murmur of the respective valve pathology. However in practice, the distinction between these areas is not that distinct. For eg., Aortic valve regurgitation produces high pitched murmur that is audible from any of the above areas.
AUSCULTATING NORMAL HEART SOUNDS :
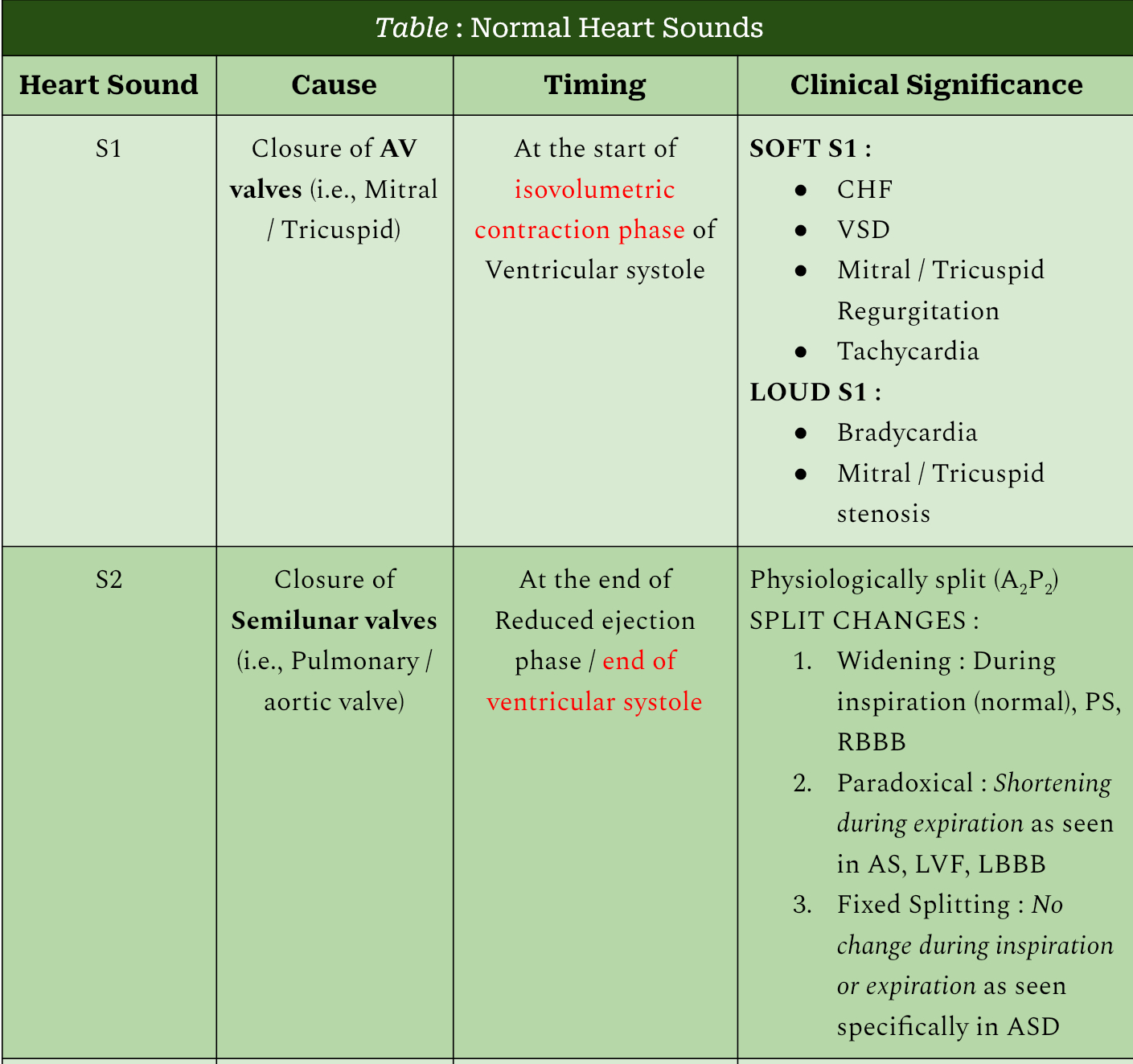
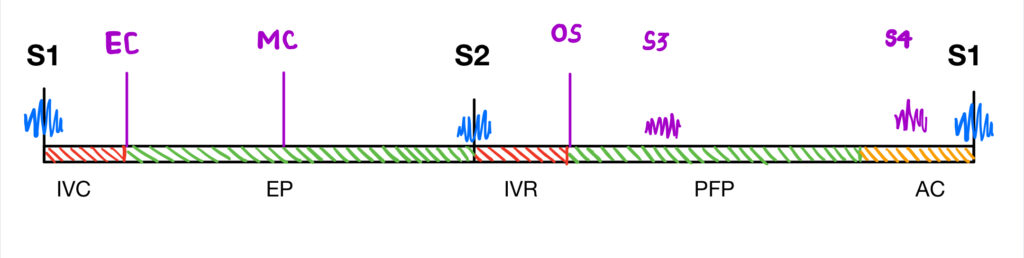
First of all, it should be made clear that by “normal”, i mean the sounds that occur during the normal cardiac cycle and no other new sounds. These “normal” sounds can very well be representative of pathology as well (eg., loud S1 or Widely split S2). I have discussed these abnormalities in the post for Heart Sounds posted earlier.
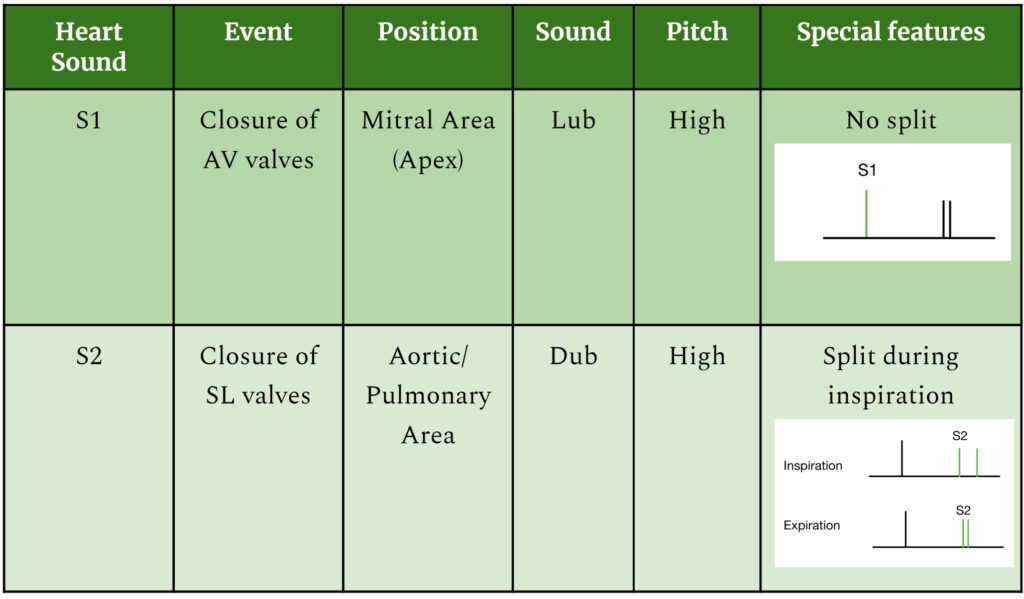
S1 and S2 can be easily recognized by their characteristic sounds “Lub…dub…lub…dub…” as in the audio given below.
If you cannot understand what these sounds mean then there are other ways to differentiate these two :
- Compare the pause in between the two sounds. Pause in between lub and dub is usually slightly shorter than the pause between dub and the next lub. Hence the correct way to identify it would be “lub..dub…….lub..dub…….lub..dub”, like that.
- S1 is louder than S2 that follows it.
- You can ask the patient to take deep breaths in order to listen to the split of S2 clearly.
It will require practice in order to differentiate these two hence one last and definite way to learn to distinguish them is to just LISTEN MORE!!
AUSCULTATING ABNORMAL HEART SOUNDS :
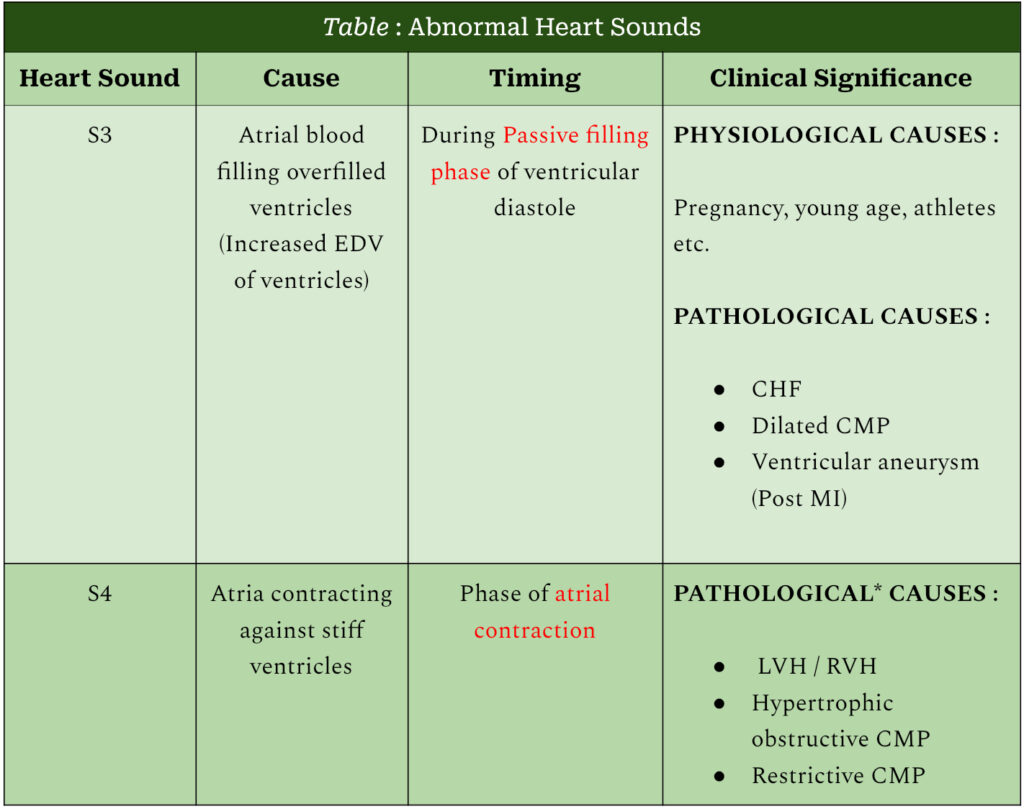
Apart from the above two sounds, a patient can have abnormal heart sounds which are result of some pathology or can be physiological as well. Details of the conditions that cause these sounds are discussed in the post covering Heart Sounds.
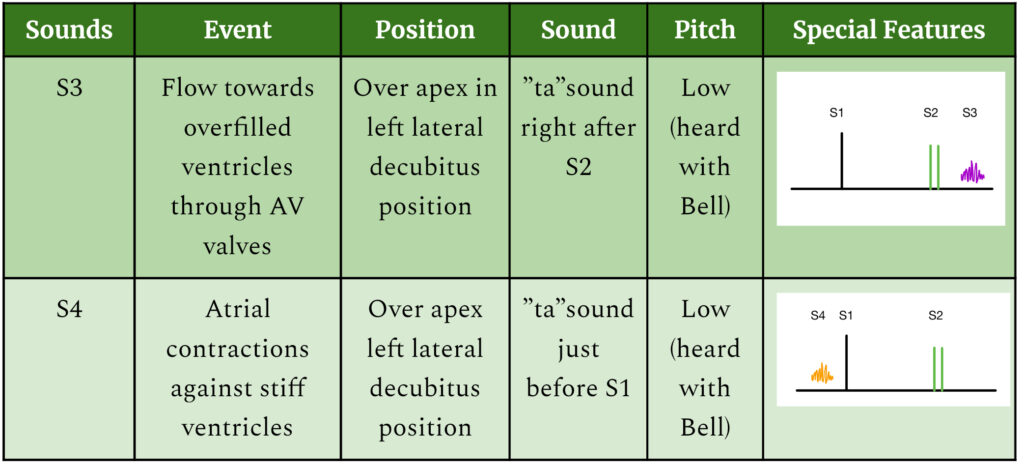
S3 when heard over apical area with the bell in left decubitus position goes like “lub…dub.ta……lub…dub.ta……lub…dub.ta”, like that.
S4 when heard in similar fashion, will be heard as “ta.lub…dub…..ta.lub…dub……ta.lub…dub”.
A genuine query arises while listening to S3 which is, “How to differentiate it from very similar sounding split S2, especially in cases of wide S2 split?”
It can be addressed in two different ways :
1). Practically it is not difficult to differentiate these two as their listening areas and parts of the stethoscope from which they are heard is completely different.
S3 : Left lateral decubitus position in apical area with bell
S2 split : Aortic / pulmonary area with diaphragm
2). In case an audio clip is given in the exam, then one would have to rely largely on the history and rest of the physical examination given such as co-morbidities, signs of heart failure, whether the audio is recorded while performing deep inspiration and expirations or not etc.
This sums up everything that you need to know in order to get started in auscultation of normal and abnormal heart sounds. Off course it is important to know the causes of abnormal heart sounds which are discussed in the other post by us. Do check that out before heading away.
SUMMARY AND STEPS OF EXAMINATION :
So once you are ready with your expensive stethoscope, take following steps in order to perform cardiac auscultation :
1). Check the functioning of the stethoscope.
2). Explain the procedure to the patient with pointing out the areas where you are going to auscultate.
3). Keep patient in sitting position at the start.
4). Listen these areas in order : Mitral – Tricuspid – Aortic – Pulmonary
(Mnemonic : Multiple Types Are Present)
5). S1 and a soft S2 are heard at apical(mitral) position. Denote any change in the intensity of S1. Rule out the causes accordingly.
6). S2 split is more appreciable in aortic / pulmonary areas and during inspiration. Note any changes in the normal split of S2. Rule out the causes accordingly.
7). Move the patient to the left lateral decubitus position and note any abnormal heart sounds in the apical area. If present, rule out/in the causes accordingly.
Please share your reviews on the article and suggestions if any. Do share it with your peers if you liked the explanation. Tell us how we can improve in the comments. See ya later!